Jaw is an important part of craniofacial bone, which maintains the integrity of facial shape, undertakes masticatory function, and is closely related to swallowing, language, breathing and other functions. After implantation, jaw prosthesis is not only pulled by surrounding muscles, but also masticatory pressure. Therefore, the prosthesis should restore the patient’s personalized appearance, and have enough mechanical strength to ensure its stability and function in vivo. It is better to load the prosthesis as a tissue engineering scaffold with osteogenic potential. Energy cells and bone-promoting growth factors can regenerate jaw bone.

Titanium and titanium alloys are widely used in oral and maxillofacial surgery due to their excellent mechanical properties, low quality, corrosion resistance and good bone bonding ability. Titanium and titanium alloy can be used to make titanium plate, titanium mesh, retaining screw and artificial prosthesis to repair maxillofacial bone defects. Because of the complex anatomical structure and contour of the jaw, traditional techniques can not accurately prepare titanium alloy prostheses that match the morphological and biomechanical characteristics of the defect area and can complete denture restoration. Therefore, some complications often occur after surgery, leading to the failure of restoration. 3D printing technology has the potential and unique advantages of completing complex structural design and making complex structures more accurately and quickly, especially in craniofacial defect prosthesis with complex shape and structure as well as complex internal structure. Therefore, with the help of digital medical imaging technology and computer aided design software, 3D printing of titanium and titanium alloy is expected to achieve the purpose of personalized design, production and repair of jaw defects. This paper reviews the recent research of 3D printing titanium and titanium alloy in the field of jaw defect repair.
- Advantages of 3D Printing of Titanium and Titanium Alloys
1.1 Sexualized Design and Manufacture of Metals
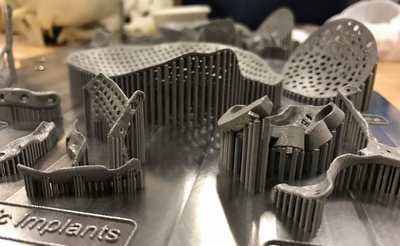
Three-dimensional printing technology includes selective laser sintering (SLS), selective laser melting (SLM) and selective electron beam melting (EBM). It uses electron beam or laser as energy source and uses computer to model three-dimensional solid parts. Through computer layered processing, it can be transformed into two-dimensional data, and then through 3D printing equipment, metal powders are melted and accumulated layer by layer to complete solid manufacturing with the advantages of high accuracy, high efficiency and low consumption.
According to the image data such as CT and the software of computer aided design (CAD), we can design the restorations which are consistent with the jaw structure and shape of the patient, and we can also design the complex structures such as porous/reticular. Making these complex restorations by metal 3D printing technology can help us to realize the jaw structure. Personalized repair. A hollow pure titanium mandibular condyle has been designed and fabricated by SLM. The condyle is not only light in weight, but also completely reconstructs the anatomical shape of the condyle, which matches the patient’s temporomandibular joint.
Chen et al. designed and applied SLM to produce two kinds of maxillary incisor implants, one is root-shaped implant and the other is root-shaped screw implant. The results show that 3D printing can design and produce root-shaped implants with high density, high strength and high precision. Root-shaped screw implants have better stress distribution, lower fretting and better quality. Good initial stability. Complex and fine structures, such as porous or three-dimensional mesh, can reduce the quality of titanium and titanium alloy restorations, and provide space for the growth of cells and blood vessels and the transport of nutrients. However, the shape of jaw is irregular, and the design of three-dimensional mesh structure is not easy, especially the topological optimization design of complex mesh structure is more difficult. Initial modeling of three-dimensional reticular scaffold for mandibular tissue engineering shows that the ideal structure of the reticular scaffold can be obtained by combining 3D printing technology with finite element topology optimization.
Mechanical Properties of Titanium and Titanium Alloys for 1.2 3D Printing
As bone tissue repair, the mechanical properties of titanium and titanium alloys are closely related to their stability, safety and osteogenic ability after implantation. The process of 3D printing technology is different from traditional metal methods such as casting, forging and powder metallurgy. Different fabrication processes will affect the structure and mechanical properties of titanium and titanium alloys. It is reported that the microstructure of forged titanium alloys is mainly coarse, plate-like or needle-like interphase beta phase, cast titanium alloys are Alpha-titanium phase, SLM titanium alloys are alpha-martensite mixed alpha phase, EBM titanium alloys are uniform needle-like alpha phase, and there are a few beta phases at grain boundaries. The Young’s modulus of titanium produced by SLS is about 104 GPa, which is close to that of forged titanium. The ultimate tensile strength and yield stress of Ti-6Al-4V made by SLM are similar to those of forging, which is superior to EBM.
The ductility of EBM is better than that of forging, SLM and casting, while that of SLM is worse. The hardness of EBM is higher than that of SLM and forged titanium alloys, while that of SLM and forged titanium alloys is similar. Fatigue strength is one of the most important properties of titanium alloy restorations. Joshi et al reported that the fatigue strength of EBM titanium alloy with vertical orientation was higher than that of horizontal orientation. After hot isostatic pressing treatment, the fatigue strength of the titanium alloy prepared by EBM is obviously improved, and the fatigue strength of the alloy is similar to that of the forged titanium alloy.
In general, the mechanical properties of titanium and titanium alloys prepared by 3D printing technology are similar to those of forged titanium alloys, but still higher than those of bone tissue. The design of porous or reticulated structure can reduce the mechanical properties of titanium and titanium alloys. Adjusting the parameters of porous or three-dimensional reticulated structure can precisely control the mechanical strength of titanium alloys and make them more compatible with bone tissue. However, such porous metals as powder metallurgy, foaming, fiber sintering and other methods can not achieve the accurate fabrication of such designs, while metal 3D printing technology can accurately fabricate complex porous or three-dimensional mesh structures with fully interconnected pores according to the design.
The stiffness and compressive strength of porous titanium alloys prepared by 3D printing decreased with the increase of porosity. Ti6Al4V implant with 61.5% porosity prepared by EBM has a compressive strength of 172 MPa and a modulus of elasticity of 3.1 GPa, which is similar to human bone tissue. By testing the mechanical properties of 3D printed reticulated titanium alloy scaffolds, it is confirmed that the biomechanical properties of the optimized reticulated titanium alloy scaffolds can meet the needs of mandibular reconstruction. However, pore structure also affects the fatigue strength of titanium alloys. It has been reported that the fatigue limit of SLM porous titanium alloys is lower than that of solid titanium alloys. Titanium alloys with different porosity have different fatigue strength, but the fatigue strength of porous titanium alloys is similar under low stress.
Therefore, according to the mechanical requirements of titanium and titanium alloy prostheses, a more reasonable stress distribution prosthesis should be designed through mechanical analysis. The mechanical properties of the prostheses should be adjusted by 3D printing technology to match the bone tissue and ensure the stable function of the prostheses in vivo. At present, the research in this field is still in progress. Very seldom.
- The experimental study of 3D printing titanium and titanium alloy in the field of jaw repair has been carried out. The stress distribution of SLM printed individualized pure titanium condylar prosthesis has been analyzed by three-dimensional finite element method. It is believed that three-dimensional printing and finite element analysis can provide a more reliable technical guarantee for the design and manufacture of temporomandibular joint repair and reconstruction. Schouman et al. used EBM to make two kinds of porous titanium metal scaffolds with different stiffness (10 times difference between high and low) to repair segmental defect of 18 mm mandible of sheep. The results showed that the amount of new bone in low stiffness porous titanium scaffolds was more than that in high stiffness scaffolds. It was believed that the growth of bone tissue could be improved by adjusting the stiffness of porous titanium scaffolds printed in However, the retaining screw of the low stiffness porous titanium alloy scaffold loosened during the experiment, which indicated that the mechanical properties of the scaffold still did not match the mandibular tissue. The study confirmed that the titanium alloy made by EBM had no effect on the proliferation and osteogenic differentiation of bone marrow mesenchymal stem cells, and had good cell compatibility. When the three-dimensional mesh titanium alloy scaffold made by EBM was used to repair the mandibular defect of Beagle dogs, it did not cause adverse reactions of the body and successfully repaired the continuity of the mandibular defect. 。 This study suggests that the three-dimensional reticulated titanium alloy scaffold made by EBM has good biocompatibility, and the three-dimensional reticulated titanium alloy scaffold is expected to be used as a bone tissue engineering scaffold to repair mandibular defects.
- Clinical study of three-dimensional printing titanium and titanium alloy in the field of jaw repairing It is our concern. According to the preoperative CT and prosthetic intention of patients, titanium mesh with thickness of 0.6 mm was made by CAD software and 3D printing equipment. Autogenous bone particles and Bio-Oss were loaded to repair the alveolar bone of maxillary atrophy. The titanium mesh only relies on its own retention, without other retention methods. After 8 months, the vertical height and horizontal width of alveolar ridge increased by 2.57 mm and 3.41 mm, respectively. After removal of titanium mesh, implants were implanted and occlusal function recovered well. Shan et al. used mirror technology and 3D printing equipment to make titanium mesh with thickness of 1 mm. Two cases of type III and V maxillary defects and two cases of mandibular chin defects caused by tumor resection were repaired with autologous fibula. All patients healed well without complications. The outline of the face was restored well.
Because the shape of the finished titanium mesh can not be completely consistent with the jaw shape of the patient, pre-bending is often required during the operation, while the pre-bending operation of the titanium mesh is difficult. In addition, after repeated adjustments, the titanium mesh is easy to fatigue, leading to fracture, and ultimately make the repair failure. The individualized titanium mesh with 3D printing is consistent with the defect area of the patient. It is easy to operate during the operation and has a good effect in the reconstruction of the jaw after the operation. It has a wide application prospect in the reconstruction of jaw. According to the patient’s CT, image technology, CAD and EBM printing equipment, individualized pure titanium guide plate, reconstructed titanium plate and titanium mesh with load-bearing plate were designed and manufactured. Four patients with mandibular defect were repaired. Individualized guide plate is used to guide the removal of jaw bone during operation, rebuild titanium plate and titanium mesh to fix vascularized fibula or free autogenous bone to repair defects. The results show that 3D printing titanium prosthesis has better operation and matching in operation and saves operation time, but the cost of 3D printing titanium metal is higher.
Suska et al. reported a case of segmental mandibular defect repaired with titanium alloy prosthesis made by 3D printing technology. The patient’s left mandible and mandibular angle were resected because of the tumors. Through the design of CAD software, a 0.8mm thick personalized titanium alloy prosthesis was made by 3D printing. The volume of the prosthesis was about 12 cm3 and the weight was 53 grams. The joint between the prosthesis and the host bone was designed as a porous structure to promote bone growth and increase the retention of the prosthesis. Six months after operation, the patient’s outline recovered well and his mental state was good.
- Summary and Prospect
Because of the complex anatomy and structure of maxillofacial bone, the design and fabrication of titanium alloy individualized prosthesis is very important. The traditional fabrication process is not only difficult to meet the requirements of accuracy, but also time-consuming and material-consuming. The 3D printing technology does not need mould, and has high precision. It saves time and material in the manufacturing process. With the rapid development of digital medicine, computer software and 3D printing technology, it is expected to realize the individualized design, manufacture and repair of maxillofacial defect prosthesis. These techniques provide great convenience for the operation and the analysis of the effect after the repair of jaw defect. It reduces the number of patients’visits, helps doctors in oral and maxillofacial surgery communicate with patients, and improves the effect of jaw repair. However, metal 3D printing technology is not perfect. Many factors will affect the performance of metal in the process of 3D printing. The printing accuracy and design of porous or three-dimensional mesh structure will have some deviations, and sometimes even print incompletely.
It is found that the micro-structure of porous titanium alloys printed in 3D has some small defects, such as sharp angle, which can easily cause stress concentration, lead to crack formation and reduce the fatigue strength of titanium alloys. Composition, printing parameters, post-processing methods and structural design of metal materials all affect the performance of 3D printing metal prostheses. There are few studies on the biological and mechanical properties of titanium and titanium alloy jaw prostheses prepared by 3D printing technology. Further studies are needed to improve the surface properties and adjust the mechanical properties. 。 At present, the technology of metal 3D printing has been used to prepare individualized titanium implants at home and abroad, but there are few animal experiments and clinical studies as jaw implants. In August 2015, the first metal 3D printing acetabular cup in China was approved by the State Food and Drug Administration (CFDA). On May 6, 2016, China’s first individualized metal 3D printing vertebral implant was approved by CFDA. However, up to now, there is no access to metal 3D printing individualized jaw prosthesis. Therefore, metal 3D printing personalized jaw implants still need further animal validation, clinical observation and strict registration review before they can be applied in clinical practice. With the development of 3D printing technology and related equipment, the cost of 3D printing of titanium and titanium alloys will gradually decrease. The application of 3D printing of titanium and titanium alloys in the field of jaw repair has great prospects.
